Introduction
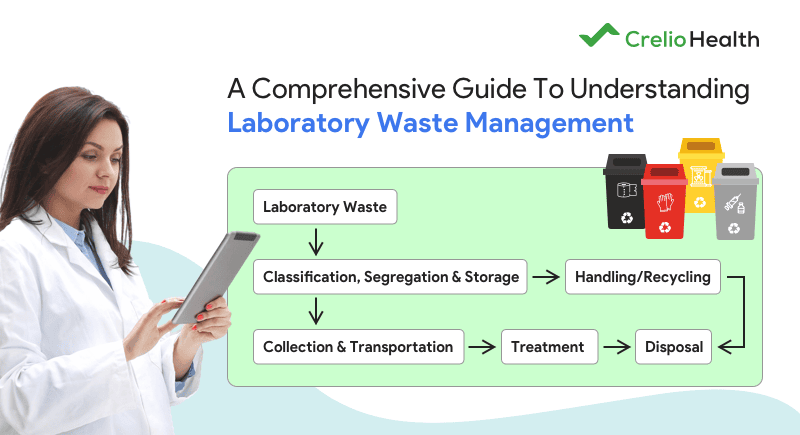
Medical laboratories generate a diverse range of waste, from biological samples to hazardous chemicals. Proper laboratory waste management and biological waste disposal in laboratory settings are critical not only for environmental protection but also for ensuring public health and workplace safety. When waste disposal is not handled correctly, it can lead to serious consequences. These include the spread of infectious diseases, chemical contamination, and regulatory penalties.
Several global standards outline essential procedures for waste management in medical laboratories. These include the WHO‘s waste management guidelines, the EU Waste Framework Directive, and NHS protocols in the UK. These regulations ensure laboratories maintain high safety and hygiene standards while reducing their ecological footprint through proper biological waste management in laboratory practices.
Table Of Contents-
1. What Is Medical Laboratory Waste?
2. Waste Characterization: Identification and Classification of Laboratory Waste
I. Importance of Classification of Laboratory Waste
II. Types of Laboratory Waste
III. Key Parameters for the Classification of Laboratory Waste
IV. Tools and Guidelines for Accurate Classification
3. Segregation of Laboratory Waste: Best Practices
I. Importance of Laboratory Waste Segregation
II. Laboratory Waste Segregation Techniques
III. Laboratory Waste Management Guidelines for Handling Specific Types of Waste
IV. Common Mistakes in Waste Segregation
V. The Role of Lab Design in Waste Segregation
4. Regulatory Standards and Compliance
I. Key Clinical Laboratory Waste Management Approved Guideline
II.Why Compliance Matters?
III. Consequences of Non-Compliance
5. Role of Staff Training in Effective Laboratory Waste Management
I. Creating Training Modules
II. Evaluating Training Effectiveness
6. Technology and Innovations Supporting Laboratory Waste Management Plan
I. Waste Tracking Systems
II. Smart Segregation Tools
III. Integration with Laboratory Information Systems (LIS)IV. Future Trends
7. Case Studies and Real-world Examples
Conclusion
1. What Is Medical Laboratory Waste?
Medical laboratory waste refers to all discarded materials generated during diagnostic testing, research, and other laboratory procedures. These materials are typically generated during the processing, testing, or analysis of biological samples, chemicals, and medical instruments. Properly identifying and handling medical laboratory waste is crucial for ensuring the safety of lab workers, patients, and the environment.
To implement an effective laboratory waste management plan, it is crucial first to understand the different types of laboratory waste. Each category requires specific handling, storage, and disposal methods to prevent hazards. Below are the key classifications of medical laboratory waste:
2. Waste Characterization: Identification and Classification of Laboratory Waste
Proper waste characterization is crucial in clinical laboratory waste management. Labs ensure safety and compliance by accurately identifying and classifying different types of laboratory waste. Hazardous materials are handled safely. These are disposed of according to regulatory guidelines. This process safeguards laboratory staff. It also helps protect the environment and the public from the harmful effects of improper waste disposal.
I. Importance of Classification of Lab Waste
The primary challenge in laboratory waste management is the need to correctly identify and classify hazardous from non-hazardous waste. Failure to follow biomedical waste management classification protocols could result in unsafe disposal practices, risking environmental harm and public health.
Effective classification of laboratory waste is crucial. All types of laboratory waste are handled and disposed of according to their level of danger. This process helps to maintain safety standards and ensure compliance with laboratory waste management guidelines.
II. Types of Laboratory Waste
Medical laboratories generate a variety of waste types, each requiring specific disposal methods. Proper waste management in laboratories begins with sorting waste into the following types:
A. Infectious Waste
Infectious waste, also known as biohazardous waste, contains pathogens that can cause diseases. Examples include:
- Used swabs, culture plates, and microbial specimens from diagnostic procedures.
- Contaminated PPE (gloves, masks, lab coats) from handling infectious materials.
- Discarded blood, body fluids, and tissues from clinical tests and research.
- Waste from patients in isolation with contagious diseases.
This type of waste must be treated using autoclaving, incineration, or chemical disinfection before disposal to eliminate biological hazards. Biological waste management in laboratory settings is highly regulated to prevent disease outbreaks and ensure safe biological waste disposal in laboratory environments.
B. Non-Infectious Waste
Non-infectious waste refers to materials that do not pose an immediate health risk. While they may not be hazardous, they still require proper segregation of biomedical waste to improve sustainability. Examples include:
- Office paper, lab notebooks, and packaging materials used in administrative tasks.
- Plastic and glass containers from non-contaminated reagents.
- General waste from break rooms (e.g., food wrappers, disposable cutlery).
By separating non-infectious waste from hazardous waste in laboratory settings, laboratories can significantly reduce their disposal costs and environmental impact.
C. Hazardous Chemical Waste
This includes hazardous chemicals that are toxic, flammable, corrosive, or reactive. Proper chemical waste classification and chemical waste segregation are essential to ensure safe handling and disposal.
- Strong acids and bases (e.g., sulfuric acid, sodium hydroxide).
- Toxic solvents and reagents (e.g., formaldehyde, xylene, chloroform).
- Heavy metals (e.g., mercury, lead, cadmium from stains and reagents).
- Explosive or reactive chemicals (e.g., peroxides, azides, cyanide).
Improper disposal of hazardous chemical waste can lead to serious environmental contamination and legal penalties. Labs must follow laboratory waste segregation in medical laboratories guidelines to prevent dangerous chemical reactions.
D. Radioactive Waste
This waste includes any material contaminated with radioactive isotopes used in diagnostic imaging, radiation therapy, and research. Examples include:
- Radio-pharmaceutical waste from nuclear medicine procedures.
- Contaminated equipment and PPE used in radiation labs.
- Liquid radioactive waste from analytical testing.
Radiation exposure poses long-term health risks. Therefore, laboratory hazardous waste management of radioactive materials must comply with strict regulatory requirements. These requirements ensure proper containment and disposal.
III. Key Parameters for the Classification of Lab Waste
To ensure proper classification of lab waste, labs must check its physical form, chemical makeup, and any potential biological risks. They should assess:
- Physical state – Is the waste solid, liquid, or gaseous? Laboratory liquid waste management requires different handling than solid waste.
- Toxicity – Does the waste contain harmful chemicals, carcinogens, or biohazards?
- Reactivity – Can the waste cause dangerous reactions, explosions, or gas release?
- Biohazard level – Does it contain infectious agents that require special handling?
By analyzing these parameters, laboratories can accurately identify types of laboratory waste. They apply the appropriate disposal methods. These methods include using SDS (Safety Data Sheets) for chemical waste. They also follow laboratory waste management SOPs for biological waste.
IV. Tools and Guidelines for Accurate Classification
To stay compliant, labs must follow standard resources and processes. These are part of the steps in waste management in laboratory settings that ensure safety and consistency:
- Safety Data Sheets (SDS): SDS provides detailed information on chemical hazards, safe handling, and disposal procedures.
- Laboratory protocols and SOPs: Every lab should implement a laboratory waste management SOP to standardize waste identification.
- Regulatory frameworks: Several documents offer classification criteria for clinical laboratory waste management. These include the EU Waste Framework Directive, WHO guidelines, and NHS waste protocols.
- Hazard labeling systems: Labs must use GHS (Globally Harmonized System) pictograms and color-coded waste bins to simplify waste identification.
Standardized classification improves efficiency and ensures proper segregation of laboratory waste at the source.
V. Common Challenges in the Classification of Lab Waste
Despite clear guidelines, there are challenges in accurately characterizing and classifying laboratory waste. Some of these challenges include:
- Misidentification of Waste Types – Laboratory staff may incorrectly classify waste, leading to hazardous waste being disposed of improperly. For instance, biological waste may be mistaken for non-infectious waste, creating a significant risk.
- Variability in Waste Composition – Waste may vary depending on the type of procedures being carried out. This variability can make waste characterization more complicated. For example, some chemical waste may have mixed properties that require special handling.
- Manual Errors – Manual errors in identifying waste types can occur if procedures are not standardized across all laboratory staff. To address this, standardization of waste management processes and regular audits can help reduce human errors and improve accuracy.
Solutions include regular training, audits, and standardized procedures to reduce risks and support an efficient laboratory waste management plan.
3. Laboratory Waste Segregation: Best Practices
Segregation of laboratory waste properly is essential for safety, compliance, and cost control. By keeping hazardous and non-hazardous waste separate, labs reduce contamination risks and improve recycling.
I. Why Segregation of Laboratory Waste Is Important?
Effective waste segregation in Laboratory helps:
- Prevents Cross-Contamination
- Enhances Recycling: Proper segregation allows for better recycling opportunities for non-contaminated materials, reducing the environmental footprint.
- Reduces Disposal Costs: Hazardous waste in laboratory settings often requires specialized handling and more expensive disposal methods. Segregating biomedical waste ensures that only the hazardous materials incur these higher costs.
- Ensures Safe Disposal: Accurate segregation prevents hazardous materials from contaminating non-hazardous waste. This ensures they are disposed of safely. Disposal is done in compliance with clinical laboratory waste management approved guidelines.
For example, a study found that 20-30% of healthcare waste classified as hazardous was actually non-hazardous, significantly increasing disposal costs. Implementing proper segregation of biomedical waste could cut these costs while ensuring safety.
II. Laboratory Waste Segregation Techniques
To streamline waste management in laboratory, a structured approach to segregation is necessary. The following methods help labs properly categorize waste and prevent accidental disposal errors:
A. Color-coded bins for Different Types of Laboratory Waste
Follow WHO and NHS standards for color coding of waste disposal in the laboratory to ensure proper segregation:
- Red bins – Infectious waste (e.g., blood-contaminated items, microbial cultures).
- Yellow bins – Sharp waste (e.g., needles, scalpels, glass slides).
- Blue bins – Non-hazardous recyclable materials (e.g., uncontaminated plastic and paper).
- Black bins – General waste (e.g., food wrappers, administrative waste).
- White bins – Pharmaceutical waste (e.g., expired medications, vaccine vials).
B. Clear Labeling to Prevent Mix-Ups
Each bin should include simple text and pictograms. This helps prevent mix-ups, especially between chemical and biological waste. Using clearly labeled laboratory waste disposal containers ensures proper segregation and safer handling throughout the lab.
C. Strategic Placement of Waste Bins
Proper placement of lab waste disposal bins is essential for efficient waste handling. Bins should be:
- Placed near workstations where waste is generated.
- Easily accessible without obstructing workflow.
- Clearly separated to prevent confusion between waste types.
Using well-placed laboratory waste disposal bins helps reduce mistakes and keeps daily lab operations safe and efficient.
III. Laboratory Waste Management Guidelines for Handling Specific Types of Lab Waste
Different types of lab waste require specialized handling to reduce risks and comply with laboratory hazardous waste management protocols.
A. Sharps Waste
- Must be disposed of in puncture-resistant laboratory waste disposal containers to prevent accidental injuries.
- Containers should be rigid, leak-proof, and clearly labeled for sharps disposal.
- Never overfill containers—sharps should not exceed the three-fourths full mark.
B. Chemical Waste
- Must be stored in sealed, corrosion-resistant containers to prevent spills or toxic fumes.
- Chemical waste segregation is critical—mixing incompatible chemicals (e.g., acids and bases) can cause dangerous reactions.
- Use secondary containment trays to minimize spill risks and comply with chemical waste classification standards.
C. Biological Waste
- Must be autoclaved, chemically disinfected, or incinerated before disposal to eliminate infectious agents.
- Liquid biological waste (e.g., blood, cultures) should be collected in leak-proof containers and processed before disposal.
- Waste tracking documentation should be maintained to monitor disposal compliance.
Proper handling reduces exposure risks and supports laboratory hazardous waste management.
IV. Common Mistakes to Avoid in Waste Segregation
Even with a laboratory waste management SOP in place, errors can still occur. Watch out for:
A. Disposing of Biomedical Waste in General Trash
- Placing infectious waste (e.g., blood-soaked materials) in regular bins can spread contamination and increase disposal risks.
- All biomedical waste must be disposed of in color-coded bins as per laboratory waste segregation guidelines.
B. Failing to Follow Laboratory Hazardous Waste Management Protocols
- Chemical waste should never be poured down the sink unless explicitly approved by laboratory waste disposal regulations.
- Radioactive waste must be stored separately from biological or chemical waste to prevent unintended exposure.
C. Mixing Chemical and Biological Waste
- Combining hazardous chemicals with infectious biological waste can cause toxic fumes or dangerous chemical reactions.
- Laboratories must ensure separate waste streams and train staff on proper segregation of laboratory waste protocols.
By addressing these common mistakes, labs can significantly improve waste disposal efficiency and safety.
V. Lab Design’s Role in Waste Segregation in Laboratory
A well-structured laboratory waste management plan should consider lab design to facilitate efficient waste disposal. Key design elements include:
A. Strategic Waste Station Placement
- Waste disposal stations should be positioned along workflow pathways to encourage compliance.
- Specialized disposal areas for chemical, biological, and radioactive waste prevent cross-contamination.
B. Designing Pathways for Safe Waste Movement
- Separate pathways for hazardous and non-hazardous waste transport reduce accidental exposure risks.
- Waste transport routes should minimize interaction with laboratory workstations to prevent accidental contamination.
Leading research laboratories have specific systems in place. They implement dedicated waste collection rooms with restricted access. This ensures the safe storage and transport of laboratory waste.
Investing in a structured segregation system ensures regulatory compliance. It also provides a safer, more sustainable, and cost-effective waste management process for laboratories worldwide.
4. Regulatory Standards and Compliance
Adhering to laboratory waste disposal regulations and compliance guidelines is essential for managing laboratory waste effectively. Laboratories worldwide must follow established frameworks to ensure safe waste management in laboratories, minimize environmental impact, and protect public health. Non-compliance can have serious consequences, including legal action, financial penalties, and reputational damage.
I. Key lab waste disposal guidelines to follow
Several international and national agencies have established laboratory waste management guidelines to regulate waste disposal in medical laboratories. These guidelines focus on proper segregation, handling, transportation, and disposal to ensure safety, sustainability, and legal compliance.
Key Clinical Laboratory Waste Management Approved Guideline
- Reduced environmental impact – Proper waste disposal prevents contamination of soil, water, and air.
- Protection of lab workers and the public – Safe handling of laboratory hazardous waste management reduces exposure risks.
- Avoidance of legal penalties – Non-compliance can result in heavy fines and legal action.
- Improved lab accreditation – Labs that follow waste segregation in medical laboratories are more likely to pass audits and gain certifications.
A. World Health Organization (WHO) Guidelines
- Provides a framework for biomedical waste management in laboratories.
- Emphasizes waste minimization, segregation, treatment, and disposal methods.
- Recommends autoclaving, incineration, and chemical disinfection for hazardous waste.
B. United Nations Basel Convention
- Regulates trans-boundary movement of hazardous waste to prevent illegal dumping.
- Requires laboratories to track and document hazardous waste disposal.
C. European Union Waste Framework Directive (EU WFD)
- Defines waste classification, recycling, and disposal standards.
- Establishes the waste hierarchy (prevention, reuse, recycling, recovery, disposal).
- Ensures strict waste segregation in medical laboratories.
D. UK-Specific Regulations for Medical Laboratory Waste Management
- NHS Waste Management Guidelines – Sets national standards for waste segregation, color-coding, and hazardous waste handling.
- Environment Agency (EA) Regulations – Enforces safe disposal of chemical, biological, and radioactive waste.
- Control of Substances Hazardous to Health (COSHH) Regulations – Requires risk assessments for hazardous substances in laboratories.
II.Why Compliance Matters?
Following global and UK-specific clinical laboratory waste management approved guidelines ensure:
For example, in the UK, improper disposal of chemical waste segregation can result in fines of up to £250,000. It can also lead to criminal prosecution under the Environmental Protection Act. Adhering to these guidelines is not just recommended—it is legally required.
III. Why Is Proper Waste Disposal Important in a Lab Setting?
Ignoring laboratory waste management SOPs can have serious consequences, ranging from legal action to financial losses and reputational damage.
A. Legal Action Due to Improper Disposal
Failure to comply with laboratory waste disposal guidelines may lead to:
- Environmental fines and lawsuits – Labs that improperly dispose of hazardous chemical waste can face prosecution under environmental laws.
- Revocation of licenses – Regulatory bodies can shut down laboratories that fail to follow waste segregation and disposal laws.
- Jail time for severe violations – In extreme cases, mismanagement of hazardous waste can lead to criminal charges. Lab managers may face these charges.
Example:
In 2022, a UK hospital laboratory faced a fine of £100,000. The fine was for illegally dumping infectious waste in a general landfill. This act violated NHS and Environment Agency regulations.
B. Financial Penalties for Regulatory Breaches
Labs that fail to comply with clinical laboratory waste management approved guidelines can face:
- Increased disposal costs – Mishandled waste often requires specialized clean-up procedures that are more expensive.
- Fines from health and safety authorities – Regulatory agencies can impose heavy penalties for non-compliance with waste management in laboratories.
- Higher insurance premiums – Laboratories with a history of poor waste management may face increased liability insurance costs.
C. Reputational Damage Affecting Lab Accreditation
A laboratory’s reputation depends on safe and ethical waste disposal practices. Non-compliance can result in:
- Loss of trust from clients and regulatory bodies.
- Negative media coverage if environmental violations are reported.
- Failure to obtain or renew accreditation from regulatory agencies (e.g., UKAS, NHS, ISO 15189).
Example:
A private diagnostic lab in London lost its accreditation after repeated violations of waste disposal protocols. This led to a drop in patient trust. Eventually, this resulted in business closure.
By staying compliant, laboratories can protect the environment. They can also maintain workplace safety and avoid legal consequences. This ensures sustainable and responsible waste management.
5. Role of Staff Training in Effective Laboratory Waste Management
A waste management plan is only as effective as the people using it. Even the best system won’t work if staff don’t receive proper training to follow it correctly. Training helps employees understand how to segregate waste, dispose of it safely, and respond to spills or emergencies, supporting proper waste segregation in medical laboratory environments.
Regular training sessions create a culture of accountability in waste management in medical laboratories. They help staff recognize their role in keeping the lab safe. These sessions ensure compliance with regulatory standards.
I. Creating Training Modules
A well-structured staff training program should cover all key aspects of laboratory waste management guidelines. Training modules should be practical, easy to follow, and regularly updated to reflect changes in regulations and waste disposal technologies.
Key Areas Covered in Training
A. Identifying Waste Types Correctly
- Differentiating between biological, chemical, radioactive, and sharps waste.
- Recognizing hazardous vs. non-hazardous waste to ensure correct disposal.
B. Following Safe Disposal Procedures
- Proper use of color-coded bins for waste segregation in medical laboratories.
- Handling laboratory hazardous waste management in compliance with regulations.
- Lab waste disposal techniques, including autoclaving, incineration, and chemical neutralization.
C. Handling Emergency Waste Spills
- Step-by-step actions for containing chemical or biological waste spills.
- Use of personal protective equipment (PPE) and spill kits.
- Emergency response protocols to minimize contamination risks.
Training should be interactive, including demonstrations, hands-on practice, and scenario-based problem-solving to ensure staff understand and retain the procedures.
II. Evaluating Training Effectiveness
Training is only effective if staff apply what they learn. To assess the success of training programs, laboratories must implement tracking and evaluation mechanisms.
Methods to Measure Training Effectiveness
A. Regular Waste Audits
- Conduct monthly or quarterly audits to check if waste is properly segregated and disposed of.
- Identify common mistakes, such as misclassified hazardous waste or improper lab hazardous waste disposal.
- Use audit results to update training content.
B. Feedback Systems to Track Compliance Gaps
- Encourage staff to report challenges they face in waste segregation and disposal.
- Provide anonymous surveys to assess training clarity and effectiveness.
- Track compliance rates through incident reports and regulatory inspections.
A laboratory that prioritizes continuous learning and process improvement will have safer waste management practices. It will also face lower compliance risks. Additionally, it will offer a healthier working environment.
Investing in staff training helps laboratories ensure long-term success in waste management. It reinforces a culture of safety and responsibility.
6. Technology and Innovations Supporting Laboratory Waste Management Plan
Advancements in technology are transforming laboratory waste management in laboratories, making waste handling more efficient, accurate, and environmentally friendly. An innovative laboratory waste management plan is backed by digital tools, automation, and AI-powered waste classification. It helps laboratories improve waste segregation, tracking, and disposal compliance. By adopting such waste management solutions, laboratories can enhance safety, reduce errors, and minimize environmental impact.
I. Waste Tracking Systems
Traditional lab waste management often relies on manual logs, increasing the risk of errors and regulatory non-compliance.
Digital waste tracking systems provide a more accurate and efficient approach by:
- Recording waste generation,classification of laboratory waste, and disposal in real-time.
- Automatically flagging hazardous waste in labs to prevent mishandling.
- Ensuring compliance with clinical laboratory waste management approved guidelines through automated documentation.
For instance, many UK laboratories now use barcode-based tracking for hazardous and biomedical waste. This method reduces incorrect classification errors by up to 30%.
II. Smart Segregation Tools
A well-planned AI and IoT-enabled tools enhance modern waste segregation in medical laboratories. They detect and sort waste with greater accuracy.
- IoT-enabled waste bins – Equipped with sensors that detect incorrect waste disposal, alerting staff in real-time.
- AI-powered waste classification – Uses image recognition and machine learning to categorize biological waste, chemical waste, and radioactive waste correctly.
- Automated bin systems – Reduce cross-contamination risks by guiding lab staff to dispose of waste in the correct waste containers.
For example, AI-based waste segregation tools have been shown to improve waste sorting accuracy by over 90% in pilot studies.
III. Integration with Laboratory Information Systems (LIS)
- A Laboratory Information System (LIS) can be integrated with waste tracking systems to:
- Monitor real-time waste disposal activities.
- Automatically generate compliance reports for regulatory audits.
- Provide alerts for improper waste handling or segregation mistakes.
By linking waste management data with the clinical LIS system, laboratories can streamline reporting. They can also reduce human error and ensure strict adherence to disposal protocols.
IV. Future Trends
The technology-backed laboratory waste management plan is constantly evolving, with exciting future trends including:
- AI-driven waste characterization – AI will enhance waste identification and classification to reduce disposal errors and improve recycling efforts.
- Sustainable disposal technologies – Innovations include waste-to-energy solutions. They also involve biodegradable waste processing and chemical neutralization techniques. These innovations will reduce the environmental footprint of laboratory hazardous waste management.
As digital solutions continue to advance, laboratories that embrace automated waste management strategies will achieve higher efficiency. They will also improve compliance and sustainability.
7. Case Studies and Real-world Examples
Real-world examples highlight how effective laboratory waste management strategies can lead to significant reductions in waste volume. This improved compliance, and cost savings. By adopting best practices in waste segregation, tracking, and disposal, laboratories worldwide have successfully minimized their environmental impact. Hence, enhancing safety and efficiency throughout the laboratory practice.
Case Study 1: UK-Based Pathology Lab Cuts Biomedical Waste by 30%
A large pathology laboratory in the UK faced rising disposal costs and concerns about improper waste segregation. Many non-hazardous materials were being disposed of as biomedical waste, increasing treatment expenses unnecessarily.
What They Did:
- Implemented a strict waste segregation system, using color-coded bins for biological, chemical, and general waste.
- Trained staff on proper waste disposal protocols, reducing errors in waste classification.
- Introduced digital waste tracking to monitor waste generation trends and improve segregation.
The Impact:
- Biomedical waste volume reduced by 30%, significantly cutting disposal costs.
- Compliance with UK waste regulations improved, reducing the risk of fines or penalties.
- Safer working conditions, as hazardous materials were properly handled and disposed of.
This case demonstrates how effective waste segregation in medical laboratories can reduce costs. It also ensures compliance with laboratory waste management guidelines.
Case Study 2: AI-Driven Waste Tracking in a German Research Lab
A leading research laboratory in Germany struggled with waste classification and documentation errors, leading to regulatory non-compliance issues. Manual record-keeping also made audits time-consuming and prone to inaccuracies.
What They Did:
- Deployed an AI-powered waste tracking system to automate waste classification and documentation.
- Integrated the system with their Laboratory Information System (LIS) for real-time monitoring of waste disposal.
- Used IoT-enabled waste bins to detect improper disposal in real time.
The Impact:
- Increased accuracy in waste classification, reducing identification errors by 85%.
- Improved regulatory compliance, as all waste disposal records were digitally logged and easily accessible.
- Faster and more efficient audits, saving several hours per month in manual reporting.
This example highlights how technology-driven laboratory waste management solutions can enhance compliance, accuracy, and operational efficiency.
Key Takeaways from Best Practices
From these case studies, key lessons emerge that laboratories can adopt to optimize their waste management strategies:
- Standardized waste classification prevents errors. It clearly defines types of laboratory waste. Using color-coded bins ensures waste is disposed of correctly.
- Strict adherence to disposal guidelines ensures safety and compliance. Following clinical laboratory waste management approved guidelines reduces the risk of regulatory breaches. It also prevents environmental harm.
- Technology integration enhances waste management – AI-driven tracking and LIS integration improve waste monitoring, documentation, and compliance tracking.
By learning from these real-world examples, laboratories can enhance their waste management practices. This ensures a safer approach. It also promotes sustainability and cost-effectiveness.
Conclusion
Effective medical laboratory waste management is not just a compliance requirement—it is an ethical and environmental responsibility. By following best practices in waste characterization and segregation, laboratories can ensure safe disposal, regulatory adherence, and sustainability.
Laboratories must implement a laboratory waste management SOP. They should invest in smart waste segregation technologies. Additionally, laboratories need to train staff to uphold the importance of laboratory waste management protocols. Doing so not only protects people and the planet but also enhances the overall efficiency of laboratory operations.
Optimize your lab’s waste management strategy for a safer, cleaner future!